People who live in group homes are at greater risk of contracting Hepatitis A, a virus that can cause liver failure and is sometimes fatal, according to the CDC. Because if this, the CDC recommends they get Hepatitis A vaccinations.
Hepatitis A is often preventable. Our lawyers investigate outbreaks, looking for the source and taking legal steps to hold wrongdoers accountable. We have a passion for advocating for persons with disabilities.
Case Study: Outbreak in Michigan Sickens 7
On April 24, 2013, a resident of a group home for adults with disabilities in southeast Michigan was diagnosed with hepatitis A and died 2 days later of fulminant liver failure. (When hepatitis A is not diagnosed until this stage, your lawyer should look at possible claims for negligent care, failure to provide medical treatment and failure to diagnose–these would be in addition to possible food poisoning claims.)
At this time, even though a resident died from this disease, none of the staff or other residents were vaccinated, which could have prevented additional illnesses. This is unconscionable, and again, would give rise to negligence and malpractice claims.
Four weeks later, a second resident of the same group home was diagnosed with hepatitis A.
Over the next 3 months, 6 additional cases of hepatitis A were diagnosed in residents in 4 other Michigan group homes. This was a wake-up call, and local health departments worked on giving hepatitis A vaccinations (postexposure prophylaxis (PEP)) to group home workers and residents.
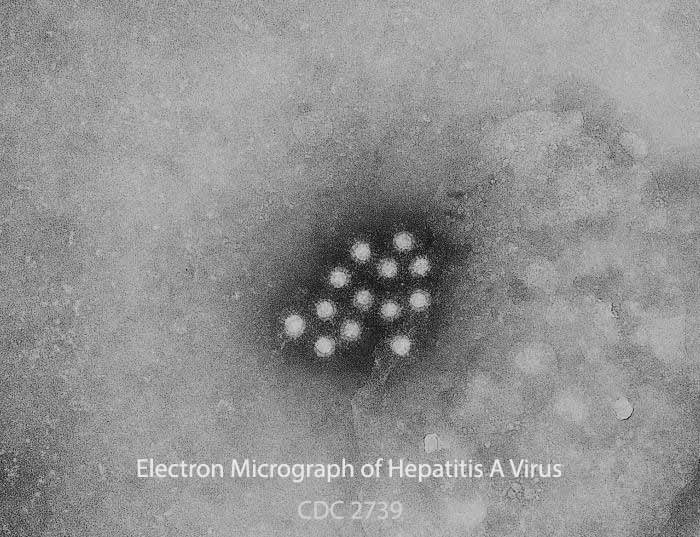
Serum specimens from 7 of the 8 cases were found to have an identical strain of hepatitis A, genotype 1A with an identical VP1/P2B genomic sequence.
Why are Group Homes High-Risk for Disease?
In most group homes, residents share rooms and bathrooms. Some require a significant amount of assistance with toileting. Sanitation with these close quarters is critical to prevent person-to-person transmission of disease, including hepatitis A.
Add to this that:
- Many of the residents of these group homes have contact with each other at work or at daycare centers; and
- Workers often work at more than one group home and/or at places were the residents are employed or taken for care during the day.
This can easily spread disease from one group home to another, as happened in this outbreak. One health care working was employed at 2 group homes and a vocational center where many residents of area group homes were employed. This person was the common link for 6 of the cases. All of these illnesses could have been prevented if the worker had been vaccinated.
None of the residents and only eight (14%) of 57 workers in the five group homes involved in the outbreak had previously received hepatitis A vaccine.
Illness onset dates ranged from April 16 to July 23, 2013. Group home attack rates, calculated as the number of cases per home divided by the number of susceptible residents, ranged from 16.7% to 60.0% among the five homes. Again, looking at the timeline of illness, it is outrageous that residents and workers throughout the area were not immediately vaccinated in April.
No common food source was identified among the five group homes. Because a multistate hepatitis A outbreak was occurring concurrently that implicated frozen berries sold at Costco and other stores, group home managers were asked if frozen berries were eaten by residents. Health officials did not find evidence that the frozen berries were consumed at the group homes or were the source of the outbreak.
The group home worker connected to 6 of the cases did not always use gloves when assisting residents with toileting, evidence of negligent care and the likely reason for transmission of serious illness to 6 people.
New Laws Needed to Protect Group Home Residents
The unvaccinated adult population in group homes is at high risk for hepatitis a virus infection, according to the CDC. Companies that own and operate group homes should be required by law to make sure all residents and workers at these facilities are vaccinated. The states need to accept the cost of these pre-exposure vaccinations as a necessary measure to prevent potentially fatal illness. These costs would be less than the expense of containing a major outbreak of illness.