The meningitis outbreak linked to New England Compounding Center (NECC) has grown to over 350 CDC-confirmed cases. According to the Massachusetts Department of Public Health (MDPH), NECC, a compounding pharmacy licensed in MA, acted like a regular drug manufacturer by selling methylprednisolone acetate (the drug implicated in the outbreak) and other drugs in bulk without individual prescriptions.
According ot MDPH, NECC distributed large batches of compounded sterile products directly to facilities apparently for general use rather than requiring a prescription for an individual patient. Records show that NECC had lists of potential patient names but did not have patient-specific prescriptions from an authorized practitioner when compounding and dispensing medication.
 Because NECC was manufacturing and distributing sterile products in bulk, it should have been licensed as a drug manufacturer with the FDA instead of a pharmacy with the Massachusetts Board of Registration in Pharmacy, according to MDPH. If it the company had done so, it would have been subject to additional levels of scrutiny.
Because NECC was manufacturing and distributing sterile products in bulk, it should have been licensed as a drug manufacturer with the FDA instead of a pharmacy with the Massachusetts Board of Registration in Pharmacy, according to MDPH. If it the company had done so, it would have been subject to additional levels of scrutiny.
It appears that NECC illegally sold the methylprednisolone acetate responsible for the fungal meningitis outbreak. This has several legal consequences, one of them is that the clinics and hospitals that used the illegal drugs are more likely to be held liable (legally responsible) for personal injury and wrongful death connected with NECC drugs.
What is a Compounding Pharmacy?
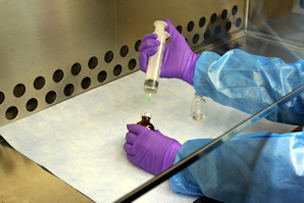
Compounding pharmacies make custom drugs for individual patients upon receipt of a valid prescription for the individually identified patient from a licensed doctor or other medical practitioner. Legitimate compounded drugs are generally exempt from key provisions of the Federal Food, Drug, and Cosmetic Act, and therefore most FDA regulation, inspection and enforcement.
In the FDA Pharmacy Compounding Compliance Policy Guides Manual, the agency suggests that certain “compounding pharmacies” act more like drug manufacturers and may be held to the same provisions of the Federal Food, Drug, and Cosmetic Act as manufacturers, including needing FDA approval for new drugs and to manufacture the drugs under conditions that ensure sterility and patient safety:
FDA believes that an increasing number of establishments with retail pharmacy licenses are engaged in manufacturing and distributing unapproved new drugs for human use in a manner that is clearly outside the bounds of traditional pharmacy practice and that violates the Act. Such establishments and their activities are the focus of this guidance. Some “pharmacies” that have sought to find shelter under and expand the scope of the exemptions applicable to traditional retail pharmacies have claimed that their manufacturing and distribution practices are only the regular course of the practice of pharmacy. Yet, the practices of many of these entities seem far more consistent with those of drug manufacturers and wholesalers than with those of retail pharmacies. For example, some firms receive and use large quantities of bulk drug substances to manufacture large quantities of unapproved drug products in advance of receiving a valid prescription for them. Moreover, some firms sell to physicians and patients with whom they have only a remote professional relationship. Pharmacies engaged in activities analogous to manufacturing and distributing drugs for human use may be held to the same provisions of the Act as manufacturers.
The FDA Guidance Manual states that when determining whether to initiate action against a compounding pharmacy, the FDA will consider whether the pharmacy engages in any of the following acts:
- Compounding of drugs in anticipation of receiving prescriptions, except in very limited quantities in relation to the amounts of drugs compounded after receiving valid prescriptions.
- Compounding drugs that were withdrawn or removed from the market for safety reasons.
- Compounding finished drugs from bulk active ingredients that are not components of FDA approved drugs without an FDA sanctioned investigational new drug application (IND) in accordance with 21 U.S.C. § 355(i) and 21 CFR 312.
- Receiving, storing, or using drug substances without first obtaining written assurance from the supplier that each lot of the drug substance has been made in an FDA-registered facility.
- Receiving, storing, or using drug components not guaranteed or otherwise determined to meet official compendia requirements.
- Using commercial scale manufacturing or testing equipment for compounding drug products.
- Compounding drugs for third parties who resell to individual patients or offering compounded drug products at wholesale to other state licensed persons or commercial entities for resale.
- Compounding drug products that are commercially available in the marketplace or that are essentially copies of commercially available FDA-approved drug products. In certain circumstances, it may be appropriate for a pharmacist to compound a small quantity of a drug that is only slightly different than an FDA-approved drug that is commercially available. In these circumstances, FDA will consider whether there is documentation of the medical need for the particular variation of the compound for the particular patient.
- Failing to operate in conformance with applicable state law regulating the practice of pharmacy.
FDA-initiated regulatory action may include issuing a warning letter, seizure, injunction, and/or prosecution.
Why Did it Take Over 300 Cases of Meningitis and 25 Deaths to Close NECC Down?
New England Compounding Center allegedly sold drugs in bulk to clinics and hospitals throughout the United States without individual prescriptions. As evidence of this and the filthy conditions of the “compounding” facility mounts, we are wondering why it took this outbreak to close NECC down. FDA sent a warning letter in 2006 regarding one drug. Apparently this did not even slow NECC down. The FDA could have seized NECC drugs illegally sold to clinics and hospitals, but it did not. It could have sought an injunction in court, but it did not. It could have prosecuted the owner and chief pharmacist Barry Cadden and others, but it did not.
The hope is that this tragic outbreak will be a catalyst for significant changes in the compounding pharmacy industry.
Attorney Fred Pritzker is representing over 40 people harmed in this outbreak. You can contact Fred for a free consultation here regarding a meningitis lawsuit against NECC, the clinic where you had your epidural injection for back pain, and others.