Hemolytic uremic syndrome (HUS) is a rare kidney disease that occurs as a complication of an E. coli O157:H7 infection. If you or a loved one developed HUS, our E. coli lawyers can help you and your family get the justice and compensation you deserve.
The Pritzker Hageman E. coli lawyers have represented people sickened in every major E. coli outbreak in the U.S. We have gone up against large companies to win some of the largest recoveries in American history.
In a landmark case, our E. coli legal team helped a little girl who developed hemolytic uremic syndrome after contracting an E. coli infection at a pumpkin patch. Read more about her family’s experience with our law firm below.

“Our Pritzker Hageman attorneys came out personally to meet with us. They took the time to sit down and talk with us and to tell us how things work. They have a real knowledge base on these types of injuries. We felt like our attorneys had a genuine concern for the well-being of our daughter in mind.”
Parent of child with E. coli-HUS
How Does Hemolytic Uremic Syndrome Cause Kidney Failure?
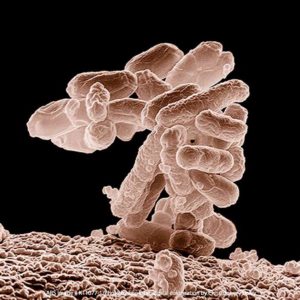
Hemolytic uremic syndrome is characterized by damage and destruction of the red blood cells, which leads to a lower than normal number of red blood cells (a condition called anemia), blood clots, and damage to blood vessel walls. HUS is primarily caused by ingesting E. coli bacteria, generally, a specific type labeled O157:H7.
Following intestinal damage from an E. coli infection, Shiga toxins created by the bacteria gain access to the bloodstream and find their way into the kidneys. There, the Shiga toxins damage the thin layer of cells that line the interior surface of tiny blood vessels in the glomerulus, which is the filtering unit of the kidney. Red blood cells are damaged and make tiny blood clots called thrombi in the filtering system. The result is kidney failure and a host of other severe medical problems.
It is impossible to describe just how horrendous this disease is. Little children can have renal failure, strokes, heart attacks, and respiratory failure. Some do not survive. This can happen with one bite of tainted food. Companies that sell that food need to be held accountable.

How Can Our Lawyers Help You?
1-888-377-8900 (Toll-Free) | attorneys@pritzerlaw.com
What are the Symptoms of E. coli and HUS?
Symptoms of an E. coli infection include:
- Bloody diarrhea, which often becomes extreme, watery, and possibly explosive;
- Severe abdominal pain
- Fever and chills, but not always
- Vomiting, but not always
The key symptom is bloody diarrhea.
The next level of illness is generally anemia, which happens because the Shiga toxins created by the E. coli bacteria have destroyed red blood cells, preventing the body’s cells from getting enough oxygen.
The first signs and symptoms of hemolytic uremic syndrome may include:
- Feeling very tired
- Unexplained weakness
- Fainting
- Paleness
If red blood cells in the kidneys are damaged, they can create small blood clots (thrombi). If this happens, the main symptom is going to the bathroom less because the kidneys are not able to make much urine. This is the primary sign and symptom of hemolytic uremic syndrome. Other signs and symptoms may include bruising and seizures.
In some cases, HUS causes acute kidney failure, signs of which include:
- Edema, which is swelling of the legs, feet, or ankles, and possibly the hands or face
- Almost nonexistent urine output
- Blood in the urine
How is HUS Diagnosed?
Please note that the CDC recommends not using antibiotics to treat E. coli infections or HUS. You should talk to your doctor about this.
You need to have a doctor make the diagnosis. Ask your doctor for one of the following:
- Urine tests
- A blood test
- A stool test to determine if there is an E. coli infection
- Kidney biopsy
In addition to testing a sample of fresh stool (feces), any dried stool around the anal area should also be tested. This is because the deadly E. coli may already have passed through the body, but the dried stool may still have traces of bacteria. It is important to both find the E. coli in the stool and then do additional genetic testing on the bacterial isolates.
This DNA testing includes pulsed-field gel electrophoresis (PFGE) and whole-genome sequencing (WGS). Not only does DNA testing help determine the illness source, but it is also evidence that can be used to get compensation for the person sickened and in some cases, that person’s family.
What are the Complications of Hemolytic Uremic Syndrome?
HUS complications are severe and can include the following:
- Kidney failure requiring hemodialysis
- Strokes
- Encephalopathy
- Acute respiratory distress syndrome
- Pancreatitis
- Diabetes mellitus
- Myocardial infarction
- Cardiomyopathy
- Cardiogenic shock
- Congestive heart failure
- Cortical blindness
- Wrongful death.
The damage done by HUS can be permanent, and patients are faced with the risk of future kidney disease. Read: “Long-term consequences of E. coli-HUS kidney failure.”
Approximately 7,500 HUS cases are diagnosed each year in the U.S. With careful and aggressive medical attention, the risk of fatality is less than four-percent.
Up to 30-percent of the children who survive the disease will be left with permanent damage to their kidneys. Children who recover usually do so quickly, while afflicted adults may experience longer recovery times since kidney damage is usually more extensive in adult cases.
Recent studies show that HUS is now the most common cause of renal failure for children in the U.S. It is recommended that people who recover undergo long-term follow-up and observation to monitor for the potential onset of chronic kidney disease, hypertension (high blood pressure), and chronic neurological damage.
Why Are Children at Risk for HUS?
Young children under 5 are at the highest risk for developing hemolytic uremic syndrome. According to some studies, as many as 15-percent of children who are infected with E. coli O157 develop HUS.
Children are more susceptible because their organs and immune systems are not fully developed. If a little one is sickened, they may end up in the hospital, on dialysis, and fighting to stay alive. Sadly, those who survive are faced with possible future kidney disease, including renal failure and the need for a transplant.
One bite of food contaminated with E. coli 0157 can do this. So can a visit to a petting zoo or interactive animal exhibit.
The Pritzker Hageman E. coli lawyers help families whose children have HUS determine:
- If their child is part of an outbreak
- What caused the illness (food, water, or animal contact)
- Who is legally responsible (food processor, restaurant, etc.)
For more information about suing on behalf of your child, see “If My Child Develops HUS from E. coli O157:H7, Should We Sue?”
Can a Pregnant Woman Develop HUS?
Yes, pregnant women are at high risk for hemolytic uremic syndrome. For example, a 26-year-old pregnant woman (31 weeks) contracted an E. coli O111 infection after eating at a restaurant (see number 6 below under the scientific literature at the bottom of this page). After 4 days, she was admitted to the hospital with extremely bloody diarrhea and severe abdominal pain.
Upon admittance to the hospital, antibiotics were administered.
The baby was delivered by C-section at 32 weeks. Although small, the baby lived.
The mother, however, went into respiratory arrest and had a heart attack (cardiac arrest). Her resulting Glasgow Coma Scale score was 11. She was diagnosed with HUS and put on hemodiafiltration and plasma exchange therapy.
The damage to her brain was significant. She had diffuse brain cortex damage and acute encephalopathy. When she emerged out of a coma on the 14th day after the C-section, she had to have rehabilitation to recover motor and cognitive functions.
Can Our Family Sue for HUS Kidney Failure from an E. coli Infection?
Yes, your family can sue if your child’s illness can be linked to a food product, a meal at a restaurant, deli, or cafeteria; or a visit to a petting zoo. Children are most at risk for developing this complication, and they have legal rights. You can sue a corporate wrongdoer on behalf of your child and make sure your son or daughter has the finances needed for a lifetime of medical expenses caused by the sale of unsafe food.
In a recent trial, Pritzker Hageman law firm won $7.55 million for a child with hemolytic uremic syndrome (HUS) who lost 50% of her kidney function and is predicted to require dialysis and kidney transplantation in her early twenties.
Hemolytic Uremic Syndrome Lawyers Help Children and Adults
Our hemolytic uremic syndrome lawyers know how to handle the unique legal issues involved with these cases. We will work to make sure you and your child are fully compensated and that future financial needs are covered. We will also work to postpone payment of medical bills until there is settlement money available.
“Acute hemolytic uremic syndrome is generally caused by ingesting food contaminated with E. coli O157:H7 bacteria. I have had clients, some of them little children, who suffered kidney failure, stroke, heart attack, and pancreatitis. More needs to be done to prevent this devastating illness.”
Attorney Eric Hageman

Filing a Lawsuit for Compensation May Be the Only Way to Get Justice
Unlike most countries, the U.S. government generally does not press criminal charges against corporate CEOs and other executives for selling tainted products. This makes filing a personal injury or wrongful death lawsuit even more important. This is often the only way to get any justice.
Our law firm is one of the very few in the U.S. that regularly represents clients, both children and adults, in these cases. Some of our clients have gone on to be food safety advocates, working to make legislative changes and educate the public about foodborne illness. Our E. coli-HUS lawyers regularly speak to various audiences about food safety.
Read more: “America’s Food Safety Law Firm.”
Outbreak News
November 2024 Minnesota Outbreak Linked to Burgers sold at Henhouse Eatery and Red Cow Restaurants
An E. coli outbreak linked to ground beef distributed by Wolverine Packing Company to Red Cow, Henhouse and other Restaurants has sickened people in Minneapolis, St. Paul and Rochester, MN.
2024 Outbreak Linked to Onions on McDonalds Burgers
An outbreak linked to slivered onions served on McDonalds Quarter Pounder cheeseburgers has sickened over 100 people and led to the death of at least one person. At least four people were sickened with HUS in this outbreak.
2024 Outbreak linked to Ground Beef used at Flathead, Montana Restaurants
Waygu ground beef sold to multiple restaurants in Flathead County, Montana is the source of a deadly E. coli O157:H7 outbreak that includes at least 14 illnesses and one death.
A 2024 E. coli outbreak has been linked by the CDC to Raw Farm Brand Unpasteurized Cheese
Raw Farms brand cheese, of Fresno, CA has been linked to 11 cases of E. coli poisoning. Two people have been diagnosed with hemolytic uremic syndrome (HUS). Cases have been identified in California, Colorado, New Jersey, Texas and Utah. Cases were first identified in October, 2023 and have continued through at least February, 2024.
Michigan, Ohio, India and Pennsylvania are Experiencing a Serious E. coli Outbreaks That Has Been Linked to Romaine Lettuce Served at the Wendy’s Hamburger Chain
Two E. coli outbreaks that had been growing throughout June, July and August of 2022, one in Ottawa County, Michigan and one in Wood County, Ohio were connected by the CDC on August 17th. additional cases also started showing up in Pennsylvania and India. Further epidemiological investigation has indicated that there is a link between this now large multi-state outbreak and the consumption of romaine lettuce served at Wendy’s restaurants within the region. The outbreak has led to serious disease and hospitalizations for many people. As of August 22nd, Michigan has reported at least 43 confirmed cases and Ohio has reported 19 confirmed cases. Many more cases may yet be discovered. Two children in the Ottawa County outbreak are believed to have developed HUS.
E. coli O26 Outbreak Linked to Cargill Ground Beef
Seventeen people were sickened in an E. coli O26 outbreak linked to Cargill ground beef, according to the CDC, whose investigators “determined that raw ground beef was the probable source of the reported illnesses,” according to a statement by the USDA. One person died. Cargill Meat Solutions of Fort Morgan, Colo. recalled about 132,606 pounds of ground beef products. The recalled products have the establishment number “EST. 86R” inside the USDA mark of inspection. They were shipped to retail locations nationwide. Meijer, Safeway, and Sam’s Club stores nationwide sold the Cargill beef before the E. coli recall. Target stores in 5 states and Publix grocery stores in Florida also sold it before the E. coli recall.
I.M. Healthy Soy Nut Butter E. coli and Hemolytic Uremic Syndrome Outbreak
An E. coli outbreak linked to I.M. Healthy SoyNut Butter products sickened at least 23 people in 9 states, including several children who developed hemolytic uremic syndrome (HUS). Two patients from the Montessori of Alameda school in Portland are part of the I.M. Healthy SoyNut Butter outbreak. Our law firm filed an E. coli-HUS lawsuit against The SoyNut Butter Company for one of the 7 children who developed HUS in this outbreak. Pritzker Hageman attorneys represented a little boy who almost died when his kidneys shut down.
Scientific Literature
Below are a few of the many articles discussing this deadly disease. Our lawyers do a lot of work in this area and keep up with the literature. You can contact our food safety legal team, led by attorney Eric Hageman, to discuss the issues raised in the articles below or your need for legal representation. Call 1-888-377-8900 (toll-free) or text 612-261-0856 to contact Eric. Because of the severity of this illness, our lawyers, upon invitation by the family, often visit clients in the hospital.
- A study looked at 259 children with O157:H7 infections, 36 of whom developed this complication. The researchers concluded that antibiotic use to treat these infections is connected to a higher rate of future HUS. Wong, Craig S., et al. “Risk factors for the HUS in children infected with Escherichia coli O157: H7: a multivariable analysis.” Clinical Infectious Diseases 55.1 (2012): 33-41 9.
- Another study concluded that the use of antibiotics may cause this complication. Smith, Kirk E., et al. “Antibiotic treatment of Escherichia coli O157 infection and the risk of HUS, Minnesota.” The Pediatric Infectious Disease Journal 31.1 (2012): 37-41.
- A higher risk of heart, kidney (renal) and pancreatic disease was found for patients who had experienced kidney failure and needed dialysis treatment. Brunelli, Steven M., et al. “Consequences of HUS among hemodialysis patients.” Journal of Nephrology 28.3 (2015): 361-367.
- This article provides a detailed discussion of the risks. This study found that most of the damage occurs in the kidneys: proteinuria [high quantities of protein in the urine]; hypertension [high blood presssure]; chronic kidney disease (CKD); and end-stage kidney disease (ESKD). Other possible health problems include: colonic strictures [narrowing of section of colon], cholelithiasis [gallstones], diabetes mellitus, or brain injury. Early dialysis lowered the mortality rate and was associated with overall better recovery and the lowering of future risks. Spinale, Joann M., et al. “Long-term outcomes of Shiga toxin HUS.” Pediatric Nephrology 28.11 (2013): 2097-2105.
- This article focuses on central nervous system (CNS) damage, often manifested by seizures and coma. CNS damage, primarily damage to the brain, is the “primary cause of death” in these patients. The center of concern in this article is hydration and its connection to CNS damage. Ardissino, Gianluigi, et al. “Hemoconcentration: a major risk factor for neurological involvement in HUS.” Pediatric Nephrology 30.2 (2015): 345-352.
- This is a case report. Ito, M., et al. “Hemolytic–uremic syndrome with acute encephalopathy in a pregnant woman infected with epidemic enterohemorrhagic Escherichia coli: characteristic brain images and cytokine profiles.” International Journal of Infectious Diseases 34 (2015): 119-121.